Pediatrics – Reflection
My pediatrics rotation at Queens Hospital Center was a wonderful experience as it exposed us to a variety of medical settings that care for the pediatric population. The first three weeks were in the pediatric emergency department. My rotation happened to land on influenza and RSV season. For this reason, the emergency department was very busy and students had a lot of opportunity for hands on experience. Furthermore, I learned to better mentally balance multiple patients at the same time while practicing how to prioritize patient care. The emergency department setting also exposed us to psychiatric consults for pediatric patients. The next week was spent at the clinic. Multiple specialists were available to care for patients that ranged from respiratory to endocrine to primary care. The work style was much different as patients were appointment-based and seen one at a time. Finally, the last week of pediatrics was spent at the NICU. This offered a rare glimpse at how hospitals take care of newborns who are premature or suffered from delivery complications.
Overall, the greatest lesson I learned in my pediatrics rotation is to develop trust and a collaborative approach with patients and their families. Children are especially difficult to communicate with and they are often fearful of medical instruments and providers. I learned to be patient with them, talk in a soft manner, and allow them to play with a stethoscope or gloves to ease their dispositions. Parents are also, naturally, very anxious or fearful as their children does not feel well. Medical concepts had to be explained in layman terms and multiple times to reassure the parents.
Moving forward, I plan to carry the lessons learned in empathetic communication and developing trust with patients. Although these aspects are emphasized in a pediatric patient demographic, they are transferable skills that would benefit all patient types. I would like to improve on my skills of balancing multiple patients in a calm manner. As the emergency department had a surge of pediatric patients, it was easy to become overwhelmed by the volume. I believe with experience and practice, I will be able to better balance and prioritize patient care in a calm and methodical manner.
Cover Letter
CV
Final CAT
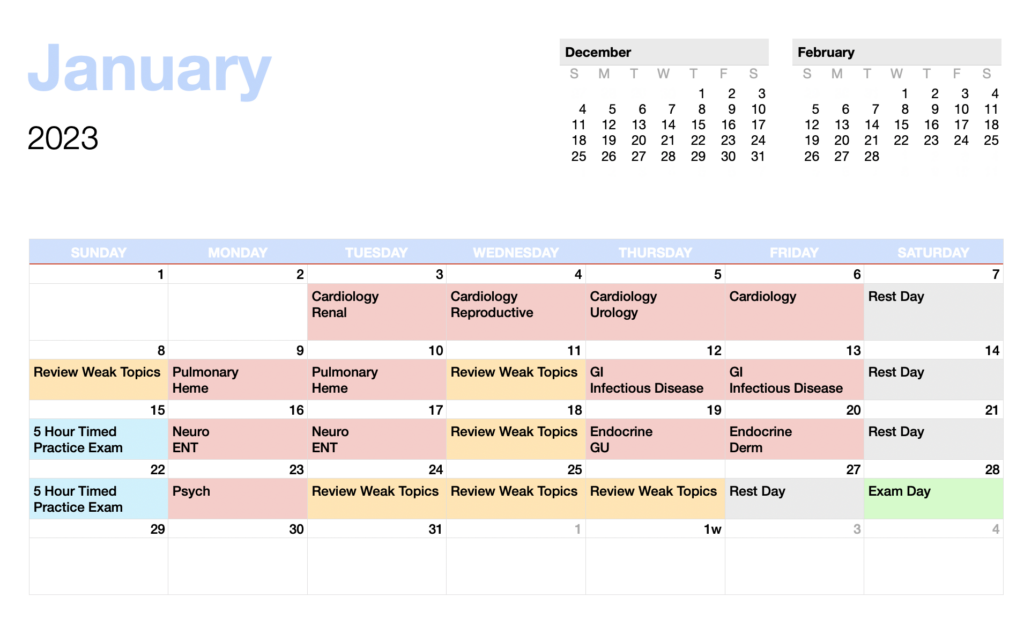
PANCE Prep Plan
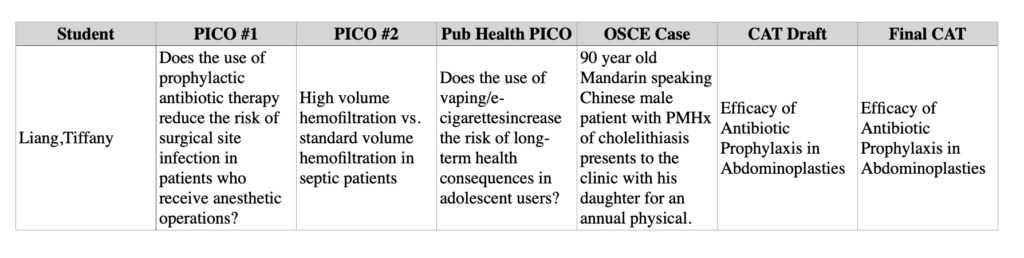
PICO/Cat Table
Pediatrics – Site Evaluation
Pediatrics – H&P
Identifying Data :
Full Name: SA
Address: Jamaica, NY
Date of Birth: 9/13/22
Age: 2 months old
Date & Time: November 10, 2022 3:30 pm
Location: Queens Hospital Center, NY
Religion: None
Source of Information: Mother & Older Sister
Reliability: Good
Chief Complaint : “Rash” x1 month and “fever” x1 day.
History of Present Illness
2 month old boy with no significant PMHx presents to the ED with his mother and older sister complaining of rash x1 months and fever x1 day. Patient’s mother explains that they took him to LIJ one month ago for a rash all over the patient’s body. They were then discharged and instructed to moisturize the patient. Mother describes the rash as “tiny red dots all over.” She explains that it appears that the baby scratches the lesions often and that the lesions have increased in number over time. She tried applying vaseline on the rash with no relief of symptoms. The family became concerned when he felt warm to touch last night. She did not give him any medications for the fever. Mother says that the baby is breastfeeding well with 5 – 6 wet diapers a day. Endorses cough. Denies vomiting, constipation, diarrhea, or wheezing. Denies sick contacts in the family. Denies recent travels.
Birth History
- Full – Term
- Vaginal delivery
- No complications
Past Medical History
- None
Past Surgical History
- None
Immunizations
- Hepatitis B
Medications
- None
Allergies
- No Known Allergies
Family History
- Mother – age 32 alive
- Father – age 34 alive, hypertension
- Sister – age 12, alive
Denies family history of cancer.
Social History
Patient is a 2 month old boy who lives in a house with his mother, father, and older sister. Mom is a stay-at-home mom and provides full care to the patient. Father works as a store manager. There are no pets in the house. No one at home smokes.
Diet : Patient eats 5 ounces every 4 hours.
Review of Systems
General – Female patient appears alert, good color, and in no acute distress. Endorses fever. Denies recent changes to appetite, constipation, and diarrhea.
Weight – Denies recent changes.
Oral Health – Denies dry mouth, swelling, bleeding.
Skin & Lymph – Endorses rash that presents as tiny red dots all over the body. Denies swollen lymph nodes, lumps, bruising and bleeding, pigmentation changes
HEENT – Denies headaches, concussions, unusual head shape, eye redness or discharge, visual problems, hearing, ear infections, draining ears, cold and sore throats, apnea, white patches on tongue, nosebleeds.
Cardiac – Denies fatigue, shortness of air, turning blue, heart murmurs, exercise intolerance, squatting, chest pains, palpitations
Respiratory – Denies wheezing, chronic cough, productive cough, coughing up blood, exposure to TB.
GI – Stool yellow-brown and runny. Denies diarrhea, constipation, vomiting, vomiting blood, jaundice, abdominal pains, colic, change in appetite
GU – 5-6 wet diapers per day. Denies blood in urine, discharge, previous infections, facial swelling.
Musculoskeletal – Denies joint swelling, injuries, or deformities.
Neuro – Denies seizures, weakness, headaches, numbness.
Pubertal – N/A
Psychiatric – Deneis difficulty sleeping, behavioral changes, hyperactivity.
Vitals
Blood Pressure – 135/60, Temp – 99.4 °F, SpO2 – 99%, Respiratory Rate – 32, Heart Rate – 159, Height – 21” Weight – 11 lbs
Physical Exam
General – Patient is a well-developed, well-nourished infant in no apparent distress. Patient is asleep but easily arousable. Appears well-hydrated.
Head – Normocephalic, atraumatic with thick hair.
Eyes – Pupils equal, round and reactive to light. Extraocular muscles appear intact but the patient is too young to cooperate with the exam. No discharge, conjunctivitis or scleral icterus. No ptosis. Patient focuses briefly on the face. Fundi-unable to visualize. Positive red reflexes bilaterally.
Ears – Clear external auditory canals. Pinnae normal is shape and contour. No pre-auricular pits or skin tags. TM’s grey bilaterally. No erythema or bulging.
Nose – Normal pink mucosa, no discharge or blood visible. Normal midline septum.
Mouth – Moist mucous membranes. No evidence of a cleft on palpation of roof.
Pharynx – Unable to visualize tonsils. Pharynx shows no erythema or ulcerations. Normal movement of soft palate.
Neck – Non-swollen. No tracheal deviation. No decrease in ROM. No lymphadenopathy, goiter or masses detected.
Chest – No increase of accessory muscles – no evidence of increased work of breathing. Lungs are clear to auscultation bilaterally. No stridor, wheezes, crackles, or rubs. Good air movement.
Cardiac: Regular rate and rhythm. Normal S1 with normally split S2 on respiration. No murmurs, gallops or rubs. 2+ pulses in all extremities including strong bilateral femoral pulses. Capillary refill less than 2 sec.
Abdomen – Soft, non-tender, non-distended. Active bowel sounds noted. No noted splenomegaly. No masses.
Genitalia – Uncircumcised; normally placed urethral meatus.
Extremities – Warm, no clubbing, cyanosis or edema. No gross deformities. Good skin turgor with no tenting. Negative Barlow and Ortolani signs.
Back – Straight, no lordosis, no kyphosis. No sacral dimple, no hair tuft.
Skin – Red-purple papular lesions 0.25 cm in diameter covering the entire body, including groin, soles of hands, and soles of feet. Some crusting and dryness noted on lesions around the thighs. No bleeding noted. Nikolsky sign – negative.
Neurological – Moves all extremities symmetrically, appropriate tone.
CN I deferred
CN II can focus on face briefly, PERRL
CN III, IV, VII unable to tell if eyes move in all directions
CN V corneal reflex deferred
CN VII symmetrical facial expression, closes eyes forcefully
CN VIII startles to clap
CN VII, IX, X, XII positive gag, symmetrical soft palate movement, normal swallow and cry
CN XI deferred
Normal symmetrical moro reflex. Upward going plantar reflexes, 2-3 beat clonus both feet.
D/Dx :
- Herpes Simplex Virus – produces fever and blisters that typically appear around the mouth and eyes. Although the red color and vesicle-like quality matches the presentation of the patient, the patient presents with vesicles all over the body.
- Hand, Foot, Mouth Disease – would present with red vesicles on the hand, foot, and mouth. However, the patient has papules all over his body.
- Roseola Infantum – usually occurs 6 – 36 months of age. Although the rash appears similar in description, the rash in roseola typically appears after fever breaks. This differs from the patient’s presentation.
- Milia – presents with small, pearl-colored cysts on the face. The patient’s rash extends all over his body and are on the soles of his hand and feet with makes this diagnosis less likely.
- Candidiasis – is often a dermatologic concern in infant patients. However, this skin infection is typically centered around the groin/diaper area. This condition should be considered but the presentation of the patient’s rash does not match and makes this differential least likely.
Assessment
2 month old boy with no significant PMHx presens to the ED with his mother and older sister complaining of rash x1 months and fever x1 day. Physical exam is positive for red papules all over the body with some crusting. Papules are also present on the soles of his hands and feet. Fever caused by infectious disease is likely. Plan is to admit the patient and transfer to hospital with dermatology and infectious disease department for continued monitoring and treatment.
Problem List & Plan
- Labs
- CBC
- CMP
- Procalcitonin
- Urinalysis
- Urine Culture
- Blood Culture
- Genmark
- Covid
- Transfer for Admit
- Admit patient for continued monitoring and treatment
- Transfer patient to a hospital with dermatology and infectious disease department
- Patient Counseling
- Advise mother to schedule remaining vaccines
- Explain the transfer process so that patient has accessibility to dermatology and infectious disease specialists

